Male Breast Surgery Scar: How the Grade of Gynecomastia Affects Scarring
One of the most frequently asked questions by patients considering male breast surgery is, “What will the scar look like?” The answer depends largely on the grade of gynecomastia, which determines the surgical technique—and therefore, the resulting scar.
At Evita Clinic, we customize the surgical plan to achieve the best results while minimizing scarring. Below is a detailed breakdown of male breast surgery scars according to gynecomastia grade (1 to 4).
Grade 1 Gynecomastia: Minimal Tissue, No Excess Skin
Surgical Approach: Periareolar incision with or without liposuction
Patients with Grade 1 gynecomastia have small amounts of glandular tissue and no noticeable skin excess. In these cases, a small semicircular incision is made along the lower half of the areola. If needed, liposuction is added through a tiny hidden port near the armpit.

-
Scar Visibility: Very subtle, often blends into the natural border of the areola.
-
Incision Size: About 2–3 cm.
-
Healing Time: Fast recovery; scars may fade almost completely within several months.
This is the least invasive form of male breast surgery, with the smallest and least visible scars.
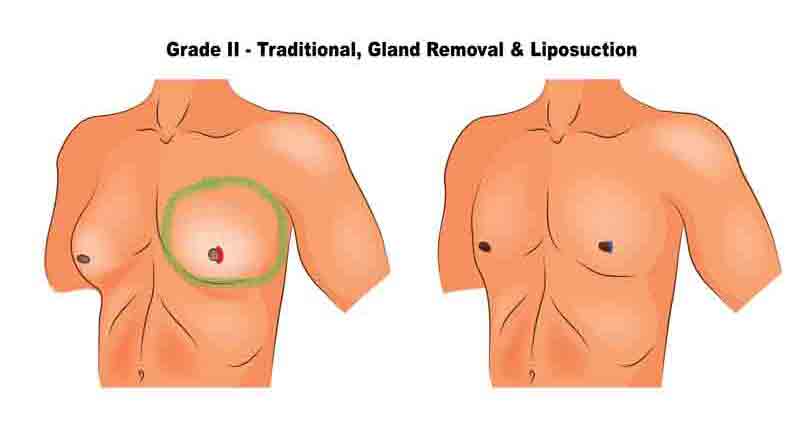
Grade 2 Gynecomastia: Moderate Gland with Minimal Skin Redundancy
Surgical Approach: Usually periareolar minimal incision; donut resection in select cases
Patients with Grade 2 gynecomastia have a moderate amount of glandular tissue and possibly mild skin laxity. However, at Evita Clinic, we typically opt for the least invasive approach whenever possible—especially if the patient is younger and has good skin elasticity.
-
In most cases, we perform a small periareolar incision, similar to the method used in Grade 1.
-
Only when the skin shows signs of reduced elasticity, such as in older patients or those with long-standing gynecomastia, do we consider a circumareolar (donut) resection.
-
Scar Visibility: Often minimal and well-concealed along the lower border of the areola.
-
Scar Shape: Semicircular in most cases; circular if donut method is used.
-
Healing Tips: Scar tension is low with the minimal approach, but compression and hydration therapy are still important to ensure smooth healing.
Even with Grade 2 gynecomastia, many patients can benefit from the minimal-scar technique, depending on age and skin condition.
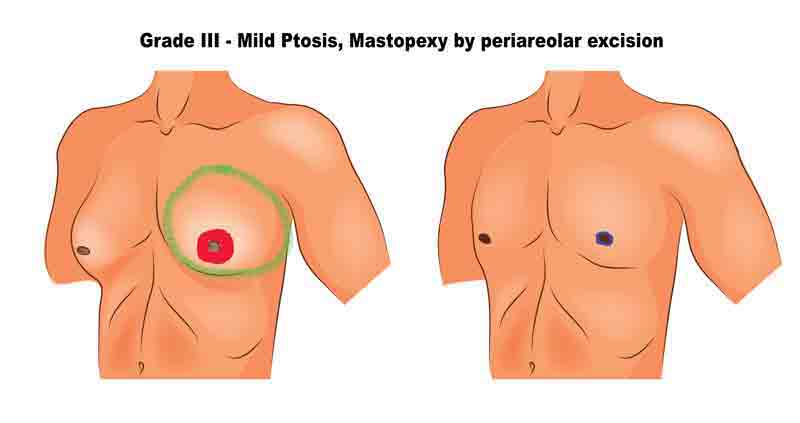
Grade 3 Gynecomastia: Large Volume with Noticeable Skin Excess
Surgical Approach: Circumareolar (donut) incision or lollipop incision, depending on skin quality
Patients with Grade 3 gynecomastia have a significant amount of glandular tissue and visible skin redundancy. The choice of surgical method in this stage depends heavily on the elasticity of the skin and the patient’s age.
-
In many cases, especially in younger patients with moderately stretched skin, we use a circumareolar (donut) incision to remove excess gland and tighten the surrounding skin.
-
However, for older patients or those with poor skin elasticity, a vertical incision extending from the areola down to the chest fold (lollipop incision) is often necessary. This allows for more effective skin removal and reshaping of the chest contour.
-
Scar Visibility: Varies—donut incisions leave scars limited to the areola, while lollipop incisions result in longer vertical scars.
-
Nipple Management: Nipple may be repositioned depending on tissue droop.
-
Healing Process: Longer than Grades 1–2, and regular follow-up is essential to monitor scar maturation.
The surgical method for Grade 3 gynecomastia is chosen based on both the severity of tissue and the quality of skin, aiming to balance contour results with scar minimization.
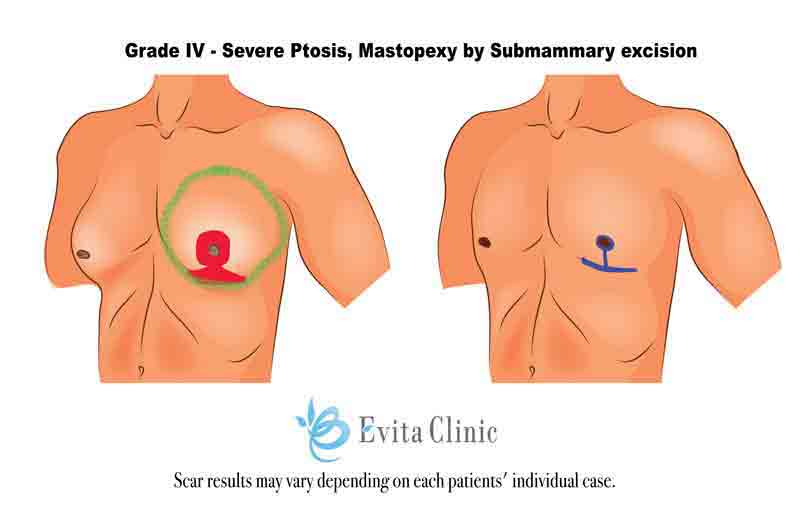
Grade 4 Gynecomastia: Severe Glandular Hypertrophy with Major Ptosis (Sagging)
Surgical Approach: Primarily anchor incision; rarely double incision with free nipple graft
Grade 4 gynecomastia is the most advanced form, characterized by massive glandular hypertrophy and severe sagging, often resembling the appearance of a female breast. These cases require comprehensive surgical correction, addressing both volume and significant skin redundancy.
-
In most cases, we perform an anchor-shaped incision—a combination of a circular cut around the areola, a vertical incision down to the inframammary fold, and a horizontal incision along the chest fold. This allows for maximum skin excision and chest reshaping.
-
In rare and exceptional cases, when the nipple position is extremely low or when skin retraction is insufficient, a double incision with free nipple grafting may be necessary. This involves removing the nipple-areolar complex and grafting it into a new position, similar to female breast reduction techniques.
-
Scar Pattern: Anchor scar (periareolar + vertical + horizontal).
-
Scar Visibility: Most prominent among all grades, but the trade-off is a dramatic and masculinized chest contour.
-
Healing Timeline: Extended healing and scar maturation over several months; close monitoring and scar therapy recommended.
Anchor incision is the gold standard for Grade 4 gynecomastia, with nipple grafting reserved only for the most complex cases.
Final Thoughts on Male Breast Surgery Scar & Healing
While the surgical grade determines the type and location of the scar, the final appearance of a male breast surgery scar is influenced by your body’s natural healing process and how well you care for the wound postoperatively.
At Evita Clinic, we guide each patient through a comprehensive scar management plan that may include:
-
Compression garment use
-
Silicone gels or sheets
-
Laser or RF therapy if needed
-
Strict sun protection
Importantly, no two people heal the same way. Some scars may fade rapidly; others take longer. Active participation in postoperative care is essential. With the right attention and management, even more prominent scars can become faint and unnoticeable over time.


![[FAQ] Can I Have Gynecomastia Surgery and Abdominal Liposuction at the Same Time?](https://evitaclinic.com/wp-content/uploads/2025/07/gyn_tummy_same-500x383.webp)

