Understanding Breast Formation in Males
Like other mammals such as dogs and cats, human fetuses develop a “milk line”—a pair of embryonic structures from which mammary tissue arises. During fetal development, this tissue is present in both males and females. However, before birth, most of this tissue regresses. In females, some tissue remains in the chest area and develops further after birth; in males, it typically regresses entirely.
Estrogen stimulates the development of breast tissue, while androgens (male hormones such as testosterone) counteract this effect. In puberty, boys may experience a temporary proliferation of breast ducts and stromal tissue. In fact, approximately 20–30% of all adolescents undergo this transient breast tissue development due to hormonal imbalance. These changes typically regress as testosterone increases and hormonal balance stabilizes, resulting in the disappearance of the lactiferous ducts.
Gynecomastia is the benign enlargement of glandular breast tissue in males, commonly accompanied by nipple sensitivity or discomfort. It is usually caused by an imbalance between estrogen and androgens—either an increase in estrogen, a decrease in androgens, or both.

When and Why It Happens

Gynecomastia typically occurs during the following life stages:
- Infancy and Puberty: Due to natural fluctuations in hormone levels.
- Aging: As testosterone levels decline, the estrogen-to-androgen ratio may increase.
- Medication Use: Certain drugs can alter hormonal balance.
- Health Conditions: Disorders affecting hormone production or metabolism can contribute.
Although people often categorize hormones as either “male” or “female,” both sexes produce estrogen and androgens. Gynecomastia results from a hormonal shift — either due to physiological changes (e.g., puberty, aging) or external influences (e.g., medication, substances).
Men and women are alike. We should not be divided based on the color of our skin. We should be one no matter our sex, race, character, and health. Like a rainbow – it consists of different colors but works beautifully together.
Persistent Pubertal Gynecomastia
Estrogen during Pubertyabout 38%
- Affects approximately 38% of adolescent boys.
- Most common between ages 10 and 16 (Tanner Stage 3).
- Triggered by an initial estradiol surge, followed by rising testosterone levels.
- Usually resolves within 6 months, but may persist for up to 2 years in about 25% of cases.
Medication-Induced Gynecomastia
Medication10 ~ 25%
Common Drugs Involved:
- Spironolactone (diuretic)
- Anti-ulcer medications: Omeprazole, Cimetidine, Ranitidine
- Anti-androgens: Finasteride
- Substances: Alcohol, marijuana, essential oils (e.g., tea tree, lavender), HAART (HIV therapy)
- Anabolic steroids and muscle-enhancing supplements: Frequently used in bodybuilding to increase muscle mass, but they can disrupt hormonal balance by suppressing natural testosterone production and increasing estrogen levels
These medications and substances may increase estrogen levels or decrease androgen activity, contributing to the development of gynecomastia. If the condition is believed to be caused by medication, the first step in treatment is to immediately discontinue the suspected drug under medical supervision.
Other Causes
Decreases testosterone10 ~ 25%
- Idiopathic (unknown) (Based on clinical experience, this is actually the most commonly observed cause.)
- Obesity: Increased fat tissue leads to higher aromatase activity, converting androgens to estrogens.
- Aging: Natural decline in testosterone.
- Hereditary Aromatase Excess Syndrome
- Androgen Insensitivity Syndrome
Diagnostic Evaluation
A proper diagnosis involves:
- Detailed History: Onset, duration, medications, systemic symptoms.
- Physical Examination: Inspection and palpation of breast tissue.
- Hormonal Testing: Blood work to assess hormone levels.
- Imaging: Ultrasound or mammography, when necessary.
Treatment Options
- Address Underlying Cause: Discontinue offending medications or treat hormonal disorders.
- Medications:
- Tamoxifen (20 mg/day): Shown to reduce breast pain and volume in ~66% of patients.
– However, due to various side effects, these cancer-related agents are not commonly used for gynecomastia and are typically reserved for select patients who are not suitable candidates for surgery. - Aromatase Inhibitors (testolactone, anastrozole, letrozole, formestane): Effective in early, active proliferation phase.
- Tamoxifen (20 mg/day): Shown to reduce breast pain and volume in ~66% of patients.
Surgical Treatment
Surgery is the most effective treatment for long-standing or fibrotic gynecomastia. Indications include:
- Psychological or cosmetic distress
- Persistent breast growth or tenderness
- Suspicion of malignancy
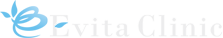
At Evita Clinic, glandular tissue removed during surgery is routinely sent for pathological examination to confirm the diagnosis. (Note: Male breast cancer is rare — accounts for only 0.5% of cases.)